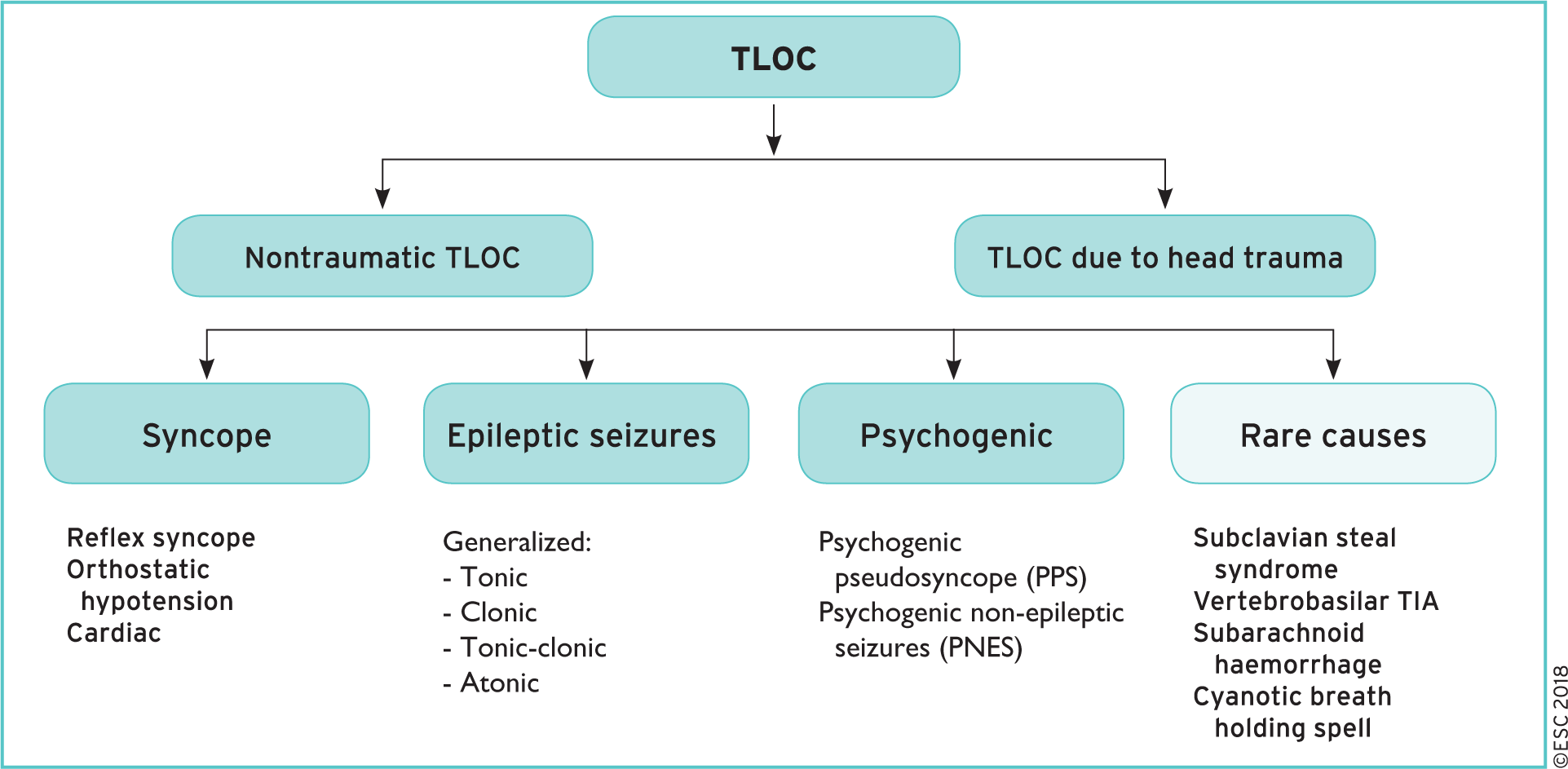
Transient Loss of Consciousness: Syncope vs Epileptic seizure
Transient loss of consciousness ('blackouts') in over 16s. NICE Clinical guideline [CG109] Last updated: September 2014
2018 ESC Guidelines for the diagnosis and management of syncope
Driving
All people who have experienced TLoC must not drive while waiting for a specialist assessment. Advise people experiencing blackouts that they may need to report this to their employer in case it affects their health and safety at work.
Definition
Syncope
Transient loss of consciousness (TLOC) due to cerebral hypoperfusion, characterized by a rapid onset, short duration, and spontaneous complete recovery.
Neurally mediated syncope (reflex syncope)
Transient loss of consciousness due to a reflex hypotensive response and/or reflex bradycardic response
Blackout
Transient loss of consciousness with complete recovery and no residual neurological deficit
Prevalence
Syncope has a lifetime prevalence of 42% up to the age of 70.
For all ages, vasovagal syncope is the commonest cause
Carotid sinus syncope and orthostatic hypotension are uncommon below the age of 40
Classification of syncope
NEURALLY MEDIATED SYNCOPE (REFLEX)
Vasovagal syncope (or faint) : triggered by pain, prolonged standing, emotional stress, instrumentation
Situational syncope such as micturition, swallow, defecation, cough, sneeze, post-exercise, laughing
Carotid sinus syndrome LoC occurred while turning the head to one side, particularly in men aged 50 years or older.
SYNCOPE DUE TO ORTHOSTATIC HYPOTENSION
Drug-induced OH (most common cause of OH): vasodilators, diuretics, phenothiazine, antidepressants
Volume depletion: haemorrhage, diarrhoea, vomiting, etc.
Primary autonomic failure (neurogenic OH): pure autonomic failure, multiple system atrophy, Parkinson’s disease, dementia with Lewy bodies
Secondary autonomic failure (neurogenic OH): diabetes, amyloidosis, spinal cord injuries, auto-immune autonomic neuropathy, paraneoplastic autonomic neuropathy, kidney failure
Other causes: adrenal insufficiency, cardiac impairment, vasodilatation (e.g. from fever)
CARDIAC SYNCOPE
Cardiac arrhythmic syncope
Bradycardia
Sinus node disease (including bradycardia/tachycardia syndrome)
AV conduction disease
SVT/VT
Long QT (corrected QT > 450 ms) and short QT (corrected QT < 350 ms) intervals.
Brugada syndrome
Ventricular pre-excitation (part of Wolff-Parkinson-White syndrome).
Left or right ventricular hypertrophy.
Structural cardiac disease
Aortic stenosis
Acute myocardial infarction/ischaemia
Hypertrophic cardiomyopathy
Cardiac masses (atrial myxoma, tumours, etc.)
Pericardial disease/tamponade
Congenital anomalies of coronary arteries
Prosthetic valve dysfunction
Cardiopulmonary and great vessels
Pulmonary embolus
Acute aortic dissection, pulmonary hypertension
SYNCOPE DUE TO POSTURAL TACHYCARDIA SYNDROME (PoTS)
Red Flags (suspected epilepsy)
A bitten tongue
Head-turning to one side during TLoC
No memory of LoC event
Unusual posturing
Prolonged limb-jerking
Confusion following the event
Prodromal déjà vu, or jamais vu
Loss of bowel and bladder control
Red Flags (cardiac arrhythmia/structural disorder)
ECG: conduction abnormality (LBBB, RBBB, heart block), long QT, ST/T abnormalities
Heart failure (history or physical signs)
TLoC during exertion/exercise
FH sudden cardiac death or inherited cardiac condition.
New or unexplained breathlessness
A heart murmur
Red Flag (cardiac or neurological or other disorder)
> 65 years who has experienced TLoC without prodromal symptoms
History
TLoC event
Patient’s activity and posture BEFORE TLoC
Any prodrome (such as sweating or feeling warm/hot)
Appearance (eyes open/closed or pallor) during TLoC
Any limb-jerking (& duration), tongue-biting
Duration of LOC
Post-LOC confusion or limb/face weakness
Was there a witness?
Past Medical History
Any previous TLoC(s)
Thee person's medical history
FH of cardiac disease or sudden cardiac death
Explore drug history (for example, diuretics)
Clinical examination
General physical examination; cardiovascular and neurological signs
Orthostatic hypotension: SBP drops by 20mmHg by 3 minutes of standing
Baseline investigations
FBC, UEs, LFTs, TFTs, glucose (+coritsol)
ECG
(CXR)
Rule out life-threatening causes for LoC
Hypogylcaemia
MI
Cardiac arrhythmia (WPW, Brugada, Long QTc (>450ms), Short QTc (<350ms), atrial arrhythmia, SVT/VT)
Pulmonary embolism
Cardiac tamponade
Concealed haemorrhage: aneurysm (AAA, thoracic aorta dissection)
Addisonian crisis: nausea, vomiting, fever, hypotension, hyperpigmentation, and electrolyte abnormalities.
Diagnosing Vasovagal Syncope (faint): no further immediate management is required
The diagnosis of reflex syncope is made when other causes of syncope are excluded and/or symptoms are reproduced in the Tilt test
There are no features that suggest an alternative diagnosis AND (the 3 'P's) such as:
Posture – prolonged standing, or similar episodes that have been prevented by lying down
Provoking factors (such as pain, emotional distress or a medical procedure)
Prodromal symptoms (such as sweating or feeling warm/hot before TLoC)
Importantly:
Brief seizure activity can occur during uncomplicated faints and is not necessarily diagnostic of epilepsy
Exercise-induced syncope: if it occurred during exercise (cardiac arrhythmic/structural disorder is likely), however, if it occurred shortly after stopping exercise (vasovagal cause is more likely).
Management
Orthostatic hypotension
Good fluid intake, extra salt if not contraindicated, compression garments, rationalisation of medication
If refectory, consider fludrocortisone, midodrine, pyridostigmine as alternatives
Referral
Referral not required if uncomplicated vasovagal syncope (faint), situational syncope or orthostatic hypertension.
All other patients experiencing a TLoC should be referred to a cardiologist or neurologist.
Additional Specialist Investigations (according to differential diagnosis)
Ambulatory ECG +/- external event recorder (if frequent TLoC)
Implantable ECG event recorder (if infrequent TLoC)
Cardiac imaging (e.g. cardiac echo test)
Carotid sinus massage test (do not perform in primary care)
Tilt Test
For people with suspected vasovagal syncope with recurrent episodes of blackout adversely affecting their quality of life, or representing a high risk of injury, consider offering referral for a tilt test to assess whether the syncope is accompanied by a severe cardioinhibitory response (usually asystole)
Definitions
Brugada syndrome An inherited ion channel disorder characterised by abnormal ST segment elevation in leads V1 to V3 on ECG. This predisposes to ventricular arrhythmia and sudden cardiac death, and may present with syncope
Carotid sinus massage A procedure in which the carotid sinus is stimulated (by firm massage with a thumb during continuous ECG and blood pressure monitoring in both supine and upright positions) to investigate suspected or possible carotid sinus syncope.
Convulsive syncope Loss of consciousness caused by transient insufficiency of blood supply to the brain accompanied by jerky or posturing movements, generally involving the limbs.
Déjà vu An intense sensation that what is happening for the first time has already occurred previously. This is common particularly in adolescence, but may be a manifestation of a partial seizure (rather than occurring immediately before an epileptic seizure).
Jamais vu A feeling of lack of familiarity, that what should be familiar is happening for the first time; it is usually abnormal, it doesn't commonly occur in healthy people.
Pseudosyncope A psychogenic non-epileptic attack characterised by loss of muscle tone and having the appearance of a faint.
Tilt test Test in which a patient is exposed to passive head-up tilt, during which they have beat-to-beat measurement of heart rate and blood pressure, to try to demonstrate whether or not they have a provocable tendency to vasovagal syncope.