Psoriasis
NICE Guideline.Psoriasis: assessment and management
Patient information leaflet: British Association of Dermatologists
Psoriasis association
Definition
Psoriasis is a systemic, immune-mediated, inflammatory skin disease which typically has a chronic relapsing-remitting course, and may have nail and joint (psoriatic arthritis) involvement.
Subtypes
Chronic plaque psoriasis (including scalp psoriasis and facial psoriasis) — also known as 'psoriasis vulgaris' and is the most common form, affecting 80–90% of people with psoriasis.
Monomorphic, erythematous plaques covered by adherent silvery-white scale, usually on the scalp, behind the ears, trunk, buttocks, periumbilical area, and extensor surfaces (such as forearms, shins, elbows, and knees).
If the scale is gently removed, a glossy red membrane with pinpoint bleeding points (Auspitz's sign) is revealed.
Occasionally, a halo-like effect is seen around a plaque, due to vasoconstriction (Woronoff's ring).
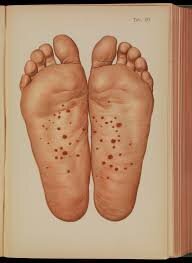
Localized pustular psoriasis of the palms and soles — the second most common form.
Flexural psoriasis — also known as 'inverse psoriasis' may affect 3–7% of people with psoriasis.
Guttate psoriasis — accounts for 2% of psoriasis cases, also known as 'droplet' lesion psoriasis, and can affect any site of the body.
Small, scattered, round or oval (2 mm to 1 cm in diameter) scaly papules, which may be pink or red.
Multiple lesions which may occur all over the body over a period of 1–7 days, particularly on the trunk and proximal limbs.
A first presentation of psoriasis (classically after acute streptococcal upper respiratory tract infection), or as an acute exacerbation of plaque psoriasis
Erythrodermic psoriasis and Generalized pustular psoriasis — (rare medical emergencies, may be life-threatening).
Nail psoriasis — affects about 50% of all people with psoriasis at diagnosis, with a lifetime incidence of 80–90%.
Nail pitting (depressions in the nail plate) is the most common finding.
It is more common in people with psoriatic arthritis (up to 90% of people have nail involvement).
Up to 10% of people with psoriasis will present with only nail manifestations.
Images (courtesy Wikimedia Commons)
Prevalence
Psoriasis is common, with about 1.3–2.2% of the UK population affected.
Predisposing factors
infection
drugs (including corticosteroid withdrawal)
ultraviolet light exposure, trauma
hormonal changes
stress
smoking
alcohol
skin trauma (Koebner phenomenon)
Associated conditions
Psoriatic arthritis
Metabolic syndrome
Venous thromboembolism
Inflammatory bowel disease (particularly Crohn's disease)
Anxiety and depression.
Differential Diagnosis
Seborrhoeic dermatitis — may mimic facial or scalp psoriasis, with greasy scale which is more diffuse and less well-defined than in psoriasis; may co-exist with psoriasis (so-called 'sebo-psoriasis').
Fungal skin/nail infection — lesions are typically either solitary, or unilateral and asymmetrical, and have central clearing with peripheral scaling.
Candidal intertrigo — may mimic flexural psoriasis, but typically presents with bright red papules, pustules, and superficial erosions with satellite lesions.
Norwegian scabies — may present with hyperkeratosis similar to that of psoriasis, with genital and axillary fold involvement.
Secondary syphilis — consider if there is palmar or plantar involvement with macules, papules, pustules, or plaques, which may mimic localized pustular psoriasis, or may mimic guttate psoriasis if lesions are more widespread.
Bacterial infection — may mimic flexural psoriasis.
Eczema — may be distinguishable from psoriasis due to lack of sharp margination. May mimic flexural or chronic plaque psoriasis, as skin can become lichenified. Chronic hand eczema can present as ill-defined psoriasis form plaques on the palms and soles.
Lichen planus — may present with mucosal involvement, scarring alopecia, severe itch, and may affect the nails.
Lichen simplex chronicus — localized areas of lichenification resulting from repeated rubbing, scratching, and itching of the skin.
Discoid lupus erythematosus — may be exacerbated by sun exposure and result in scarring.
Cutaneous T-cell lymphoma — rare; presents with itchy, red, scaly patches however, unlike psoriasis, there is colour variation among the patches.
Guttate psoriasis may present similarly to:
Viral exanthems.
Pityriasis rosea — psoriatic scale involves the whole lesion and is coarser than the finer, localized ring pattern of the scale of pityriasis rosea.
Drug eruptions.
Generalized pustular psoriasis may present similarly to:
Pyogenic infections.
Vasculitis.
Drug eruptions.
Diagnosis
Distribution — psoriasis often occurs on extensor surfaces (elbows and knees), trunk, flexures, sacral and natal cleft, scalp and behind the ears, and umbilicus.
Size and shape of lesions — there is usually a clear delineation between normal and affected skin.
Colour — may be pink or red, but in people with pigmented skin this may not be obvious. Scale is typically silvery in colour.
Involvement of other areas — such as the joints or nails or sites of trauma (Koebner phenomenon)
Medical Emergency
Generalized pustular psoriasis
Rapidly developing widespread erythema, followed by the multiple non-follicular pustules which coalesce to form large lakes of pus.
Lesions associated with systemic illness: fever, malaise, tachycardia, weight loss, and arthralgia.
Usually presents in people with existing or previous chronic plaque psoriasis, but can also occur in people without a history of psoriasis.
Erythrodermic psoriasis
Diffuse, widespread severe psoriasis that affects more than 90% of the body surface area with widespread erythema
It can develop gradually from chronic plaque psoriasis or appear abruptly, even in people with mild psoriasis
It can be precipitated by various factors such as systemic infection; irritants such as coal tar or ciclosporin; phototherapy; or sudden withdrawal of corticosteroids
Lesions may feel warm, and may be associated with systemic illness: fever, malaise, tachycardia, lymphadenopathy, and peripheral oedema
Localized (palmoplantar) pustular psoriasis
Lesions on the palms and soles, such as yellow-brown pustules within established psoriasis plaques, or redness, scaling, and pustules at the tips of the fingers and toes.
Arrange for referral to a dermatologist, the urgency depending on clinical judgement, for specialist assessment and management.
Consider seeking specialist dermatology advice whilst awaiting specialist assessment, regarding interim treatment options that may be initiated in primary care.
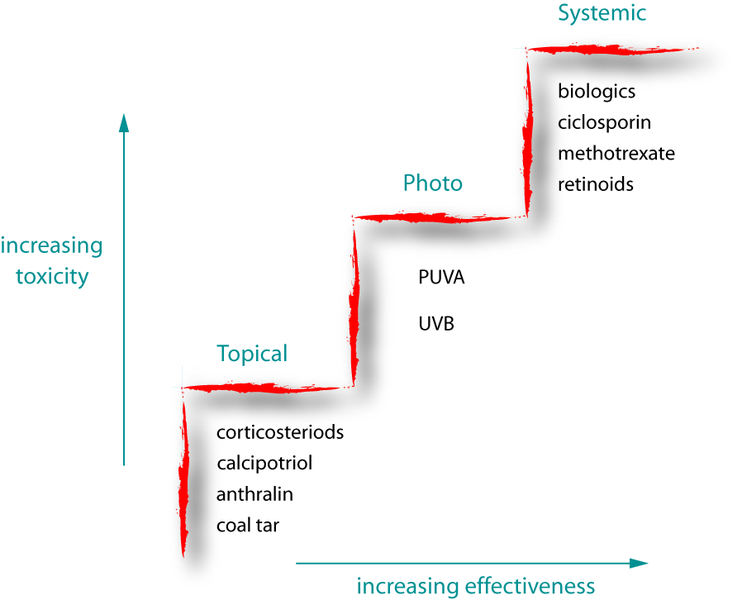
Management
Topical lesion-specific
emollients
corticosteroids
vitamin D analogues (calcitriol)
coal tar
short-contact dithranol (for large plaque psoriasis)
Phototherapy (risk of skin cancer)
narrowband ultraviolet B light (nbUVB/TLO1)
ultraviolet A light (PUVA) PLUS oral/topical psoralen (sensitiser).
Systemic treatments
Methotrexate or ciclosporin
Biologic treatments : Injectables etanercept, adalimumab, infliximab, ustekinumab, secukinumab, ixekizumab and guselkumab.
Articular symptoms of unexplained joint stiffness, pain, or swelling; or nail changes: Psoriatic arthritis
Specialist rheumatology referral
Holistic and lifestyle consideration
Lifestyle advice such as weight loss, smoking cessation, and alcohol reduction (if appropriate).
Management of associated stress, distress, anxiety and/or depression.
Assessing the risk of cardiovascular disease at least every five years, especially if psoriasis is severe.
Giving advice on how to reduce the risk of venous thromboembolism, especially if psoriasis is severe.
Referral should be arranged to a dermatology specialist
There is uncertainty about the diagnosis.
Psoriasis is extensive, for example more than 10% of the body surface area is affected.
Psoriasis is at least moderately severe.
Psoriasis is resistant to topical drug treatments in primary care, or treatments are not tolerated.
There is nail disease which is severe and having a major functional or cosmetic impact.
There is a significant impact on the person's physical, psychological, or social wellbeing.
Additional information or education for self-use is needed (for example about application of topical treatments).
Specialist treatments may include
topical calcineurin inhibitors
phototherapy (ultraviolet light therapy)
systemic or biologic (antibody) therapy