Comprehensive Geriatric Assessment (CGA)
CGA in Primary Care Settings. British Geriatrics Society. British Geriatrics Society. 28 January 2019
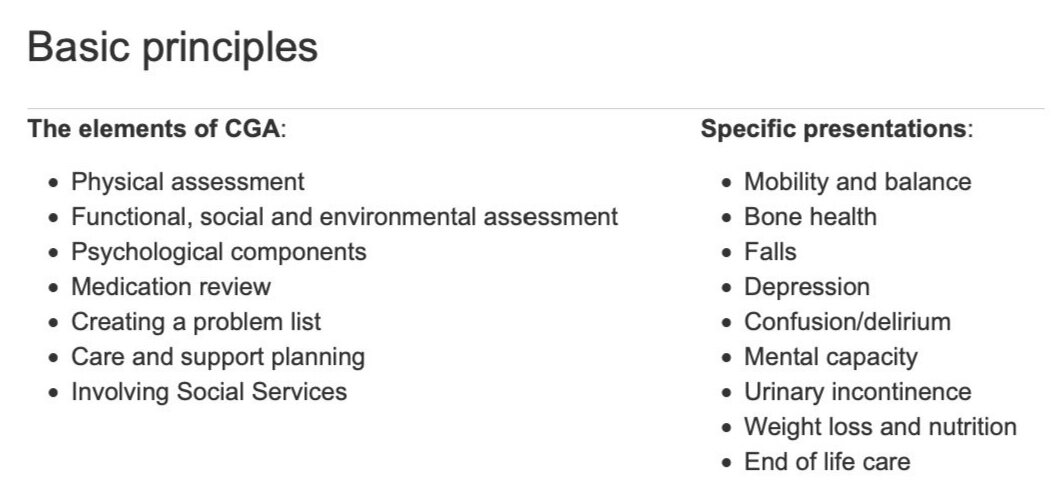
CGA Specific presentations Mobility and balance, Bone health, Falls, Depression, Confusion/delirium, Mental capacity, Urinary incontinence, Weight loss and nutrition, End of life care
CGA Toolkit for Primary Care Practitioners (pdf)
Definition
Comprehensive Geriatric Assessment (CGA), or
Comprehensive older age assessment (COAA), or
Geriatric Evaluation Management and Treatment (GEMT)
is a process of integrated care comprising a number of steps:
Multidimensional holistic assessment
Creation of a problem list to address issues
Intervention
Regular planned review
Why is it done?
Evidence shows that CGA is effective in secondary care :
reducing mortality
improving independence for older people
reducing hospital admission and readmission
reduce the impact of frailty
reverse the progression of frailty
The evidence base for primary care care is not yet as strong. A systematic review by Garrard et al (2019) concluded potential benefits
cost-effecttiveness
improved medication adherence
reduced hospital admission rate
effect on mortality outcomes were inconsistent
When is CGA done?
Presenting with frailty syndromes – i.e. falls, confusion, reduced mobility and increasing incontinence
even if these appear to be due to a reversible cause – such as a new medication or minor infectionWhen a GP or community team learns of an incident which implies frailty- for example if an ambulance is called after a fall
Discharged from hospital after presenting with a frailty syndrome (fall, reduced mobility, delirium etc) even if another diagnosis has been offered as the cause.
In care homes - most residents of care homes will have frailty.
Several tools for risk stratification and for frailty ‘screening’ are available and more are being developed, such as Electronic frailty index eFI which is embedded in System one and EMIS.
Who may be involved?
General practitioner
Community geriatrician (if available)
Community nursing team (including community matrons, dedicated nurses from the CCG, district nurses)
Physiotherapists
Occupational therapists
Community psychiatric nurses CPN
Pharmacists
The elements of the CGA process
CGA comprises interdisciplinary and interagency working in a number of domains:
Physical assessment
Sensory loss
Feet and footwear
Gait and balance: Timed up and Go Test (TUGT), number of steps to turn 180 degrees
Lying and standing BP (at 0, 1min, 3min)
Cognition and mood
Functional ability
Pain/joints
Weight and nutrition
PR and genitaliaFunctional, social and environmental assessment
Mobility
Activities of daily living, Nottingham Extended ADL Scale,
Barthel Index,
BGS Social & Environment Questionnaires
Driving
Timed up and Go Test (TUGT)
3. Psychological components: Mood and Cognition
Cognition:
Useful screening question for patient/carers:
“Has the person been more forgetful in the last 12 months to the extent it has affected their daily life? For example, difficulty using the phone, managing shopping lists, using money, managing their medication, driving, etc.
Cognitive assessment
in Primary Care
Abbreviated mental test score (AMTS)
General practitioner assessment of cognition (GPCOG) GP-Cog test
Mini-cog
Cognitive assessment
in Memory Clinics
Addenbrookes cognitive examination-III (ACE-III)
Alzheimer’s Society Practical Toolkit for clinicians
5. Creating a Problem List
Consider baseline tests and further specialist tests (e.g. 24hr ECG or colonoscopy etc).
Baseline tests:
Full Blood Count
Urea Creatinine (Chronic Kidney Disease (CKD)
Electrolytes (be aware sodium <125mM/L can cause confusion and tiredness)
Glucose
Liver Function Tests (ALP elevated with Paget’s disease or post-fracture)
Calcium
C Reactive Protein (CRP) ESR
Thyroid Function Tests
PSA
Urinalysis
Chest Radiography (CXR)
Electrocardiograph
What should a care plan include?
The diagram below summarises nine key areas that ought to be included at the end point of the CGA process as the individualised care plan for a frail older person.