Osteoporosis and fragility fractures
CKS Osteoporosis
UK clinical guideline for the prevention and treatment of osteoporosis 2017
Definition
Osteoporosis is characterised by low bone mass (measured by bone mineral density) and microarchitectural deterioration of bone tissue, with a consequent increase in bone fragility and susceptibility to fracture.
Osteoporosis itself is asymptomatic.
Fragility fracture is a fracture following a fall from standing height or less, although vertebral fractures may occur spontaneously, or as a result of routine activities.
An osteoporotic fracture is a fragility fracture occurring as a consequence of osteoporosis. Characteristically, fractures occur in the wrist, vertebrae, and hip.
Consequences of osteoporosis
The risk of getting an osteoporotic fracture depends on the person's risk of falls, their bone strength (determined by bone mineral density [BMD]), and other risk factors.
Around 25%-30% of the deaths following hip or vertebral fractures are related (directly or indirectly) to the fracture, and around 70-75% to comorbidities.
Prevalence
The prevalence of osteoporosis increases markedly, from approximately 2% at 50 years of age to almost 50% at 80 years of age. More than one in three women and one in five men will sustain one or more osteoporotic fractures in their lifetime.
Diagnosis of osteoporosis by DXA scan
Bone mineral density (BMD) is measured by dual-energy X-ray absorptiometry (DXA).
Osteoporosis is defined as a BMD T-score ≤ −2.5
The T-score is the number of standard deviations that the measured BMD is from the mean BMD of young age (30-40y, peak bone mass) and the same gender and ethnicity.
The Z-score is the number of standard deviations that the measured BMD is from the mean BMD of adults of the same age, gender and ethnicity as the test subject
Normal T-score ≥ −1.0 85% of population have a BMD above T-score -1.0
Osteopenia T-score -2.5 < T score < -1.0 14% of population will have a BMD within this range
Osteoporosis T-score ≤ −2.5 0.6% of population with have a BMD within this range
Severe Osteoporosis T-score ≤ −2.5 AND Fragility fracture
The International Society for Clinical Densitometry states diagnosis of osteoporosis:
in men under 50 years of age should not be made on the basis of densitometric criteria alone.
in premenopausal women, should use Z-scores rather than T-scores and consider other information in addition to densitometric criteria.
BMD measurement does not assess the microarchitectural structural deterioration in bone.
Consequently, most osteoporotic fractures occur in women whose BMD does not meet the criteria for osteoporosis.
Pathology
Osteoporosis is the end result of an imbalance in the normal process of bone remodelling by osteoclasts (promote bone breakdown) and osteoblasts (promote new bone formation).
Risk factors for osteoporosis
Female gender
Increasing age
Menopause
Oral corticosteroids
Smoking
Alcohol
Previous fragility fracture
Rheumatological conditions, such as rheumatoid arthritis and other inflammatory arthropathies
Parental history of hip fracture
Body mass index of less than 18.5 kg/m²
Calcium and vitamin D deficiency
Non-osteoporotic causes for fragility fracture
Metastatic bone cancer
Myeloma
Hyperthyroidism
Osteomalacia
Paget's disease
Secondary causes of osteoporosis:
oral corticosteroids
premature menopause
hypogonadism in men
diabetes mellitus
hyperthyroidism
rheumatological disorders
chronic malabsorption syndromes (such as Crohn's disease, UC, coeliac disease)
chronic liver disease
chronic renal disease
chronic obstructive pulmonary disease
Who should be given osteoporosis treatment without the need to undergo fragility fracture risk assessment?
According to NOGG guideline (2016):
Women who have had a previous fragility fracture.
People over 70 years of age who are taking high dose corticosteroids.
People with hip or vertebral fracture where assessment is considered inappropriate or impractical
Who should undergodual-energy X-ray absorptiometry (DXA) scan without the need to undergo fragility fracture risk assessment?
>50y + previous fragility fractures
<40y + major risk factor (such as steroid use, previous fragility fracture).
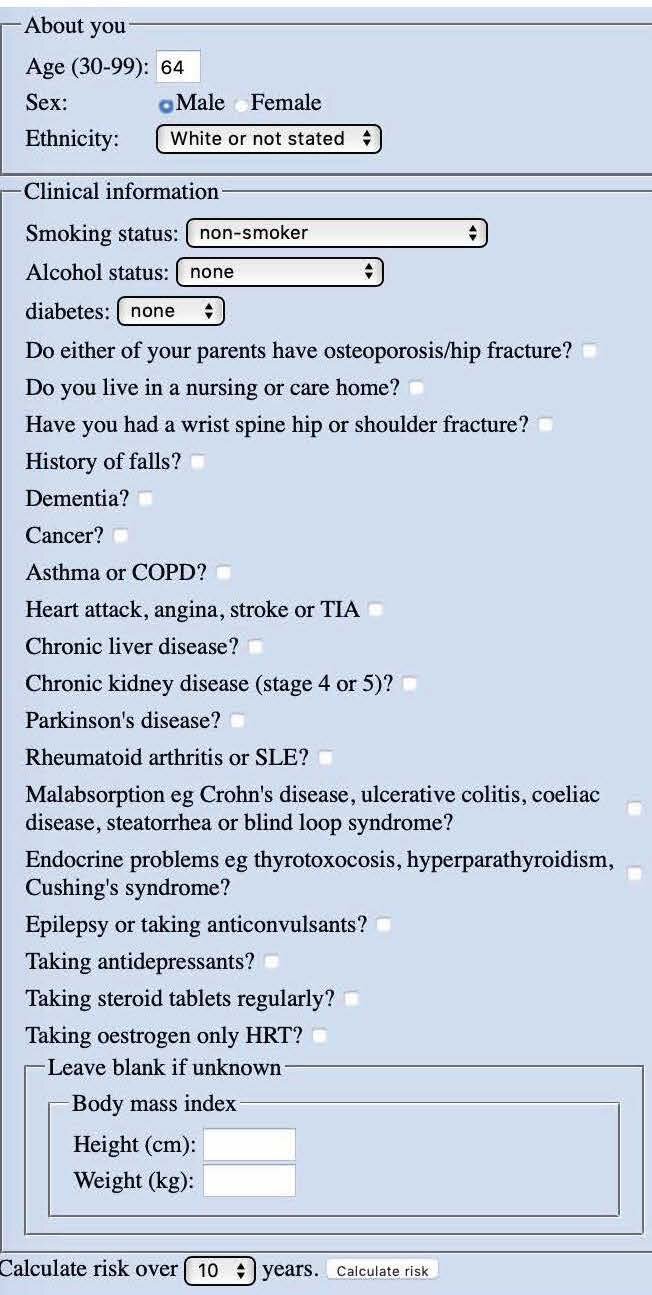
Fragility fracture risk: 10-year probability of fracture
For all other people with risk factors for osteoporosis, calculate the 10-year fragility fracture risk prior to arranging a DXA scan to measure BMD.
Fragility fracture risk should be calculated using: QFracture® (preferred) or FRAX®.
FRAX® score generates:
10-year probability of hip fracture
10-year probability of a major osteoporotic fracture (clinical spine, forearm, hip or shoulder fracture).
QFracture has additional factors which are not included in FRAX
QFracture generates:
10-year probability of hip fracture
10-year probability of a osteoporotic fracture (hip, spine, wrist or shoulder)
How to interpret a fragility fracture risk score
Note: QFracture® is high risk is >11.1% (for women) or >2.6% (for men)
People at high risk perform DXA scan
People at intermediate risk consider DXA scan
People at low risk give lifestyle advice, do not offer drug treatment or DXA scan
Treatments
Postmenopausal women and men over 50 years of age who have been confirmed by dual-energy X-ray absorptiometry (DXA) scan to have osteoporosis (bone mineral density [BMD] T-score of -2.5 or less).
Prevent bone resorption
Bisphosphonates [prevent bone resorption]
Once-daily: alendronate 10 mg once daily (M+F)
Once-weekly: alendronate 70 mg once weekly (F), risedronate 35 mg once weekly (M)
Once-yearly: zoledronic acid : i.v. 5mg WITH PRIOR Vitamin D loading (100,000 IU) AND >2w after hip fracture repair [up to 3 years duration]
Adverse effects of Bisphosphonates:
Upper gastrointestinal adverse effects, such as dyspepsia or reflux.
Symptoms of atypical fracture, including new onset hip, groin, or thigh pain
Osteonecrosis of the jaw
If bisphosphonate is not tolerated or is contraindicated:
Denosumab: s.c. 60 mg every 6 months [human monoclonal antibody that inhibits osteoclast formation via RANK Ligand inhibition]
Estradiol, estropipate, conjugated oestrogen [HRT]
Raloxifene oral 60 mg once daily for women only [selective oestrogen receptor modulator']
Teriparatide: s.c. 20mcg daily for 24 months [parathyroid hormone receptor agonist]
Vitamin D and calcium
First-line alendronate/risedronate
Then concurrent maintenance daily: 20mcg (800 IU) Vitamin D3 + 1000mg calcium
Second-line potent antiresorptive agent (zoledronate or denosumab or teriparatide)
NEED Vitamin D loading:
Approximately 50,000 IU (tablets, capsules or liquid) given weekly for 6 weeks
Then, commence maintenance vitamin D
Other treatments for osteoporosis
Hormone replacement therapy, particularly for women with premature menopause
should be managed if present.
Follow up
Adverse effects of bone-sparing treatment.
Adherence to treatment.
Need for continuing treatment with bisphosphonates after 3–5 years.