Chronic Obstructive Pulmonary Disease
Useful links
Patient information leaflets on COPD from British Lung Foundation
NICE COPD guideline July 2019
Global Initiative for Chronic Obstructive Lung Disease (GOLD) COPD Strategy
Excellent summary article (incorporating NICE and GOLD guidelines) published by The Primary Care Respiratory Society (Oct 2019)
Incidence
Known 1.2 million diagnosed with COPD in the UK, however, many more (1-2m) considered undiagnosed.
Overarching five fundamentals:
Stop smoking
Pneumococcal and influenza vaccinations
Pulmonary rehabilitation if MRC dyspnoea scale ≥3 (mMRC ≥ 2)
Personalised self-management plan
Treat co-morbidities
London Respiratory Team COPD Value Pyramid
Diagnosis
SYMPTOMS
Exertional breathlessness
Chronic cough or regular sputum production
Frequent winter bronchitis
Wheeze
*If they have a personal or family history of lung or liver disease and consider alternative diagnoses, such as alpha‑1 antitrypsin deficiency
RISK FACTOR EXPOSURE
Tobacco smoking
Occupation with exposure to chemicals or dust
AIRFLOW OBSTRUCTION
Post-bronchodilator Spirometry:
Forced expiratory volume in 1 second (FEV1)/forced vital capacity (FVC) ratio of <0.7
Reversibility testing is unnecessary and may be misleading
There can be overlap between COPD and asthma and distinguishing can be diagnostically challenging.
Recommended Investigations
Post-bronchodilator Spirometry
CXR Chest radiograph to exclude other pathologies
FBC Full blood count in case of anaemia or polycythaemia (and to check eosinophils)
BMI Calculation of body mass index.
Other specialist investigations:
Testing for serum alpha-1 antitrypsin deficiency if there is early onset (<45yr), panlobular basal emphysema, minimal smoking history, or a family history of that condition
Low concentration (<20% normal) suggests homozygous deficiency.Serial home peak flow readings to exclude asthma if diagnostic doubt remains.
Classification of severity of airflow limitation
1.Spirometry based on post-bronchodilator FEV1 in patients with FEV1/FVC <0.7
GOLD 1: mild FEV1 ≥ 80% predicted
GOLD 2: moderate FEV1 50-79% predicted
GOLD 3: severe FEV1 30-49% predicted
GOLD 4: very severe FEV1<30% predicted
2. Five level modified MRC Dyspnoea Scale grade 0 to grade 4 (+1 to each mMRC grade equates to original MRC Dyspnoea scale grade 1 to grade 5)
mMRC Grade 0 = I only get breathless with strenuous exercise
mMRC Grade 1 = I get short of breath when hurrying on the level or walking up a slight hill
mMRC Grade 2 = I walk slower than people of the same age on the level because of my breathlessness, or I have to stop for breath when walking on my own pace on the level
mMRC Grade 3 = I stop for breath after walking about 100m or after a few minutes on the level
mMRC Grade 4 = I am too breathless to leave the house or I am breathless when dressing or undressing
3.COPD Assessment Test (CAT)
Treatment
Offer the ‘five fundamentals’
Mainly breathlessness (dyspnoea) (GOLD A+B):
1st line: SABA
2nd line: SABA + (LABA or LAMA)
3rd line: SABA + (LABA and LAMA combined)
Progress from 1st—>2nd—>3rd line if there is continued breathlessness that limits daily activities (MRC≥2)
Mainly exacerbations (+/- breathlessness) (GOLD C+D):
1st line: SABA + (LABA or LAMA)
2nd line: SABA + (LABA and LAMA combined)
3rd line: SABA + LAMA + (LABA + ICS combined)
Progress from 1st—>2nd—>3rd line if there is continued exacerbations +/- breathlessness
COPD with ‘asthmatic’ or ‘steroid responsive’ features:
1st line: SABA + (LABA + ICS)
2nd line: SABA + LAMA + (LABA + ICS combined)
Consider 3-month trial of Triple therapy (LAMA + LABA + ICS) if:
Non-asthmatic COPD or asthmatic COPD limited by symptoms or has exacerbations
Elevated eosinophils
Start 3-month trial of triple therapy, and if symptoms improve, continue, otherwise revert to dual therapy
Asthma–chronic obstructive pulmonary disease (COPD) overlap syndrome (ACOS)
ACOS is estimated to be prevalent in 15–20% of people diagnosed with COPD.
Defining ‘asthmatic’ or ‘steroid responsive’ features in COPD patients:
Personal history of asthma or atopy
Elevated blood eosinophil count
Substantial variation in FEV1 over time (at least 400 ml)
Substantial diurnal variation in peak expiratory flow (at least 20%)
Evidence of clear symptomatic or lung function response to short trial of corticosteroids (oral or inhaled)
Higher (x3 times) frequency of exacerbations in people with asthma–chronic obstructive pulmonary disease (COPD) overlap syndrome (ACOS) compared to those with typical COPD alone
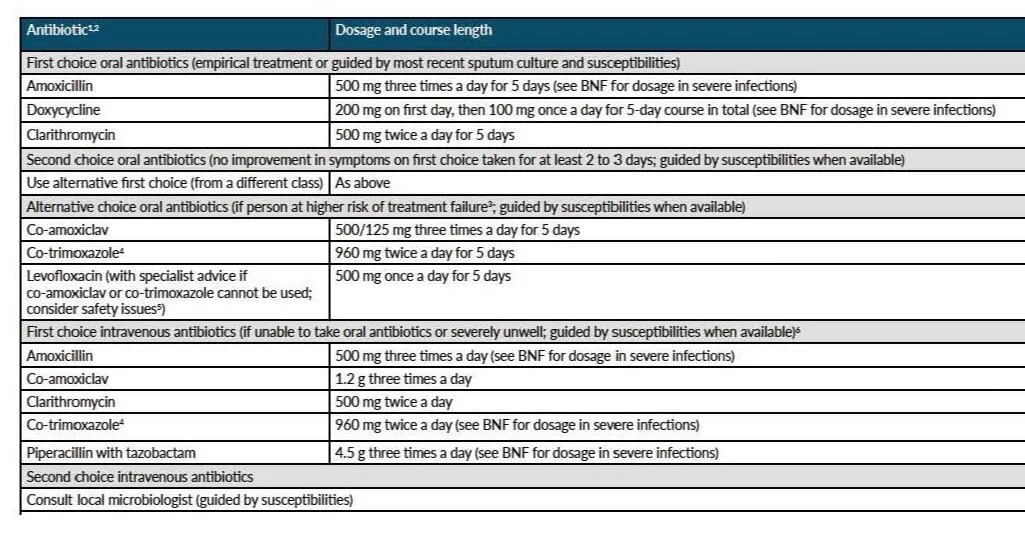
NICE COPD Antimicrobial guideline
Plan for and treat COPD exacerbations
Develop an individualised exacerbation action plan
’Rescue pack’ as part of their exacerbation action plan
5 days oral prednisolone 30mg once daily PLUS oral 5 day course of antibiotics to keep at home
However, if symptoms and signs suggest the acute exacerbation is severe, then refer to hospital.
Bronchiectasis
7–14 days antibiotic course recommended
In COPD exacerbations, with increased cough and sputum purulence, antibiotics, regardless of choice, reduce the risk of short-term mortality by 77%.
Therefore their use is supported in those who are moderately to severely ill.
Inhaled corticosteroids alone do not reduce exacerbation or reduce mortality.
Inhaled corticosteroids (alone and in combination with long-acting beta-adrenoceptor agonists or LABAs) increase the risk of pneumonia in patients with COPD.
ORAL THERAPIES
Oral corticosteroids
Long-term use of oral corticosteroid therapy in COPD is not normally recommended (risk of osteoporosis)
Oral theophylline (slow-release formulation)
Theophylline may be considered if inhaled therapies have failed or for people who are unable to use inhaled therapy
Plasma levels and interactions (such as macrolide or fluoroquinolone antibiotics) need to be carefully monitored.
Oral mucolytic therapy
Only continue mucolytic therapy if there is symptomatic improvement (feduction in frequency of cough and sputum production)
Oral prophylactic antibiotics in people with frequent exacerbations
Consider regular azithromycin therapy (usually 250 mg three times a week) following seeking respiratory specialist referral/advice.
The following criteria should have been met before starting prophylactic antibiotics:
Do not smoke
Optimised non-pharmacological management and inhaled therapies, relevant vaccinations and (if appropriate) have been referred for pulmonary rehabilitation
Continue to have frequent or prolonged exacerbations/hospital admissions
Sputum culture (including for tuberculosis), to identify other possible causes of persistent or recurrent infections
Patient has had training in airway clearance techniques to optimise sputum clearance
CT scan of the thorax to rule out bronchiectasis or other lung pathology
Specific to azithromycin: ECG to rule out prolonged QT interval and baseline liver function tests.
The person should also receive a warning about the small risk of hearing loss and tinnitus from azithromycin and be advised to contact their health professional if this occurs.
Patients who are taking prophylactic azithromycin may also keep antibiotics (different in class to azithromycin) at home as part of their exacerbation rescue pack.
It is not necessary to stop prophylactic azithromycin during an acute exacerbation of COPD.
Oral phosphodiesterase-4 inhibitors
Roflumilast, as an add-on to bronchodilator therapy, is recommended as an option for treating severe COPD with chronic bronchitis, only if:
severe as shown by FEV1<50% predicted/best, following bronchodilator
≥ 2 exacerbations in the previous 12 months despite triple inhaled therapy (LAMA+LABA+ICS)
Treatment with roflumilast should be started by a specialist in respiratory medicine.
Long-term oxygen therapy
Continuous long-term home oxygen therapy (LTOT), for a minimum 15 hours per day, can improve survival in people with COPD who have more severe hypoxaemia.
The need for oxygen therapy should be assessed in:
All patients with severe airflow obstruction (FEV1 < 30% predicted)
Patients with cyanosis, polycythaemia, peripheral oedema, raised JVP or oxygen saturations < 92% breathing air.
Assessment should also be considered in patients with moderate airflow obstruction (FEV1 30–49% predicted).
Many patients tolerate mild hypoxaemia well, but once the resting artierial oxygen partial pressure (PaO2) falls below 8 kPa patients begin to develop signs of cor pulmonale, principally peripheral oedema. Once this occurs the prognosis is poor and if untreated the five year survival is less than 50%.
Eligibility criteria:
Non-smoker
Arterial Blood gases should be measured on two occasions at least 3 weeks apart
ABG PaO2 <7.3 kPa when stable
ABG PaO2 7.3-8 kPa AND any combination of secondary polycythaemia, peripheral oedema, pulmonary hypertension.
Firm diagnosis of COPD and be receiving optimum medical management for their condition, which should be stable.
Risk assessment for long-term oxygen therapy
Any risk of burns and fires as a result of smoking while using oxygen OR falls from tripping over equipment?
People who meet the criteria for LTOT who smoke (or who live with people who smoke):
Offer smoking cessation advice and treatment,
If still smoking, do not offer long-term oxygen therapy
If not smoking but live with someone who smokes, the risk may (subject to risk assessment) may be lower
Ambulatory oxygen therapy
Ambulatory oxygen therapy needs respiratory specialist assessment before it is started.
Ambulatory oxygen can be considered for people with COPD who, on assessment by a specialist, have exercise desaturation and are shown to have an improvement in exercise capacity with oxygen; they should also have the motivation to use oxygen.
Evidence shows that neither ambulatory oxygen nor short-burst oxygen provides a clinically meaningful improvement in breathlessness for people with mild or no hypoxaemia.
Short-burst oxygen to manage breathlessness for people with COPD, who have mild or no hypoxaemia at rest, should not be offered.
Lung volume reduction surgery
The evidence for lung volume reduction (LVR) surgery or endobronchial valve replacement now shows benefit in certain individuals with COPD, with improvements in lung function, exercise capacity, quality of life and long-term mortality
At the end of pulmonary rehabilitation and at other reviews, offer a respiratory review for surgery if all the following apply:
FEV1 <50%
Quality of life is limited by breathlessness despite optimal treatment
The patient does not smoke
The patient is able to walk a distance of at least 140 metres in 6 minutes.
A specialist lung volume reduction multidisciplinary team will assess the patient’s suitability for surgery
COPD service audit targets
Ensure that all patients with COPD get access to the five ‘fundamentals’
Staff who perform or interpret spirometry are trained and certified
Check medication is correct for COPD
Offer smoking cessation treatments
Review high-risk patients, such as those using >3 rescue packs (steroids+antibiotics) per year