Management of asthma in adults and children
RightBreathe website for guidance in inhaler technique.
BTS/SIGN Guideline on Asthma (SIGN 158) July 2019
Principles
Asthma management requires optimisation of the following processes:
Pharmacological treatment
Non-pharmacological treatment
Supported self-management
Monitoring
Aim to achieve
complete control of asthma:
• no daytime symptoms
• no night-time awakening due to asthma
• no need for rescue medication
• no asthma attacks
• no limitations on activity including exercise
• normal lung function (FEV₁ and/or PEF >80% predicted or best)
• minimal side effects from medication
BTS/SIGN Asthma Guideline July 2019
BTS/SIGN Asthma Guideline July 2019
Pharmacological management
Treatment is started at the level most appropriate to initial severity, increasing or decreasing treatment until control of asthma.
Before modifying treatment, check adherence with existing therapies, inhaler technique and eliminate trigger factors.
In children, a pMDI and spacer is the preferred method of delivery of β₂ agonists and inhaled corticosteroids.
MART Maintenance and Reliever Therapy
pMDI Pressurised Metered Dose Inhaler
DPI Dry powder inhaler
SABA Inhaled short-acting β₂ agonist
ICS Inhaled corticosteroid
LABA Inhaled long-acting β₂ agonist
LRTA Leukotriene receptor antagonist (oral montelukast)
AVOID generic prescribing of inhalers: prevents people with asthma being given an unfamiliar inhaler device which they are not able to use properly.
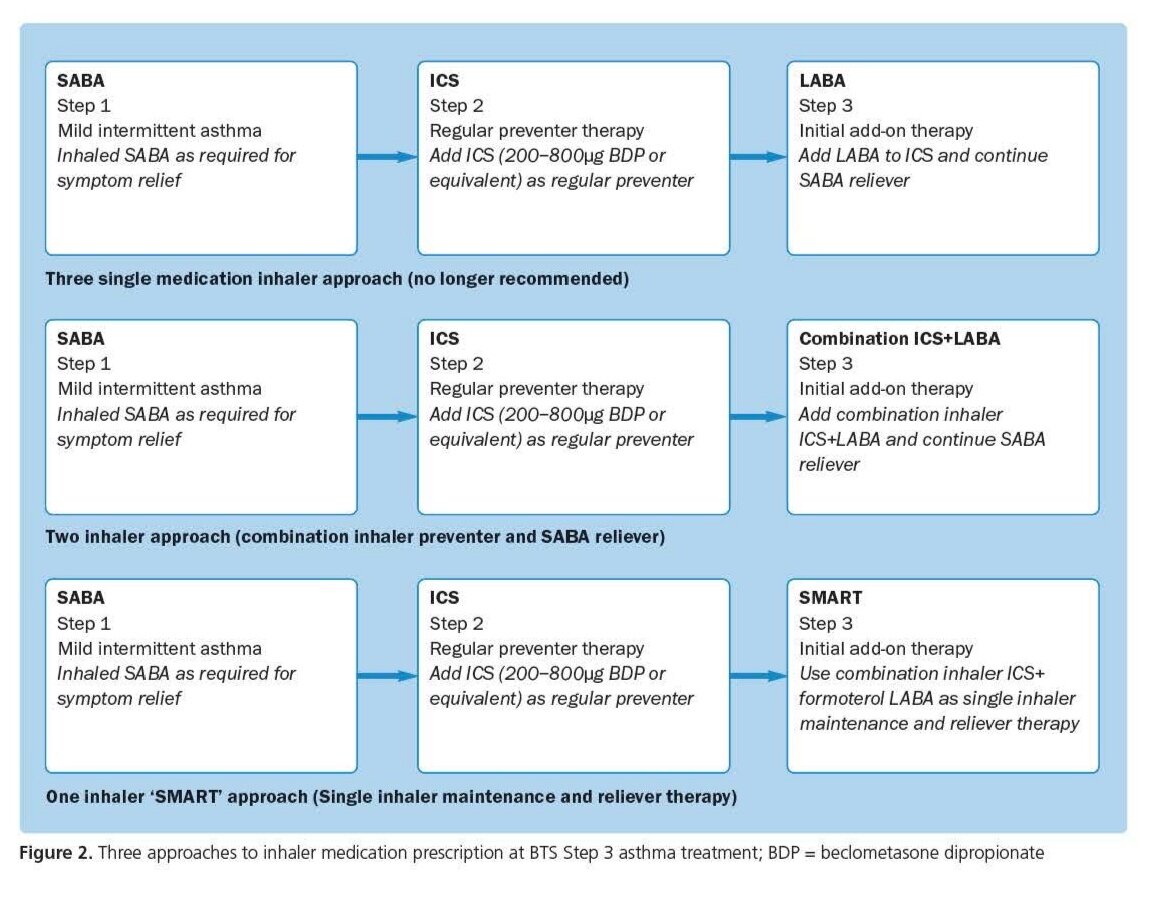
Treatment package:
Regular Preventer (maintenance) PLUS SABA reliever
or fixed-dose ICS+LABA with SABA reliever
or SMART (single inhaler maintenance and reliever therapy)
and other potential add-ons of
LTRA (montelukast)
modified-release theophylline
tiotropium (if age>12).
Spacer advice:
The spacer should be compatible with the pMDI
Single actuations of the metered dose inhaler into the spacer, followed by inhalation
Minimise delay between pMDI actuation and inhalation
Tidal breathing is as effective as single breaths
Spacers should be cleaned (detergent) monthly rather than weekly as per manufacturer’s recommendations
Mouthpiece should be wiped clean of detergent before use
Plastic spacers should be replaced at least every 12 months but some may need changing at six months.
Treatment package ADULT CHILD
1. Regular Preventer Low-dose ICS (200-400mcg BDP): initially twice daily Very low-dose ICS (or LTRA if age<5y)
2. Initial add-on Low-dose ICS+ LABA Very low-dose ICS + LABA (if age ≥5y) or LTRA (any age)
(separate LABA, combination ICS/LABA or SMART)
3. Additional controller therapy Medium-dose ICS/LABA (800mcg BDP) OR add LTRA Low-dose ICS OR add LTRA (age ≥5y) or add LABA (age ≥5y)
MART or fixed-dose ICS+ LABA with SABA reliever
4. Refer for specialist therapies
Selected preferred inhalers
Aerosol pMDI+ Spacer Dry Powder Inhaler DPI
SABA Salbutamol 100mcg Easyhaler Salbutamol 100mcg
Low-dose ICS Clenil Modulite 100mcg Easyhaler beclometasone 200mcg
Low dose ICS + LABA Fostair 100/6 Fostair NEXThaler 100/6
(<400mcg BDP) Seretide 50 Evohaler Seretide 100 Accuhaler
Flutiform 50/5 DuoResp Spiromax 160/4.5
Symbicort 100/6 and 200/6 Turbohalers
Fobumix 80/4.5, Fobumix 160/4.5
Medium dose ICS + LABA Fostair 100/6 Fostair NEXThaler 100/6
(400-800mcg BDP) Seretide 125 Evohaler Seretide 250 Accuhaler
Flutiform 125/5 DuoResp Spiromax 160/4.5
Sereflo or Sirdupla 125 Revlar Ellipta 92/22
Symbicort 200/6 and 400/12 Turbohalers
Fobumix 160/4.5
Fixed High dose ICS + LABA Fostair 200/6 Fostair NEXThaler 200/6
(>800mcg BDP) Seretide 250 Evohaler Seretide 500 Accuhaler
(plus SABA reliever) Flutiform 250/10 DuoResp Spiromax 320/9
Sereflo or Sirdupla 250 Revlar Ellipta 184/22
Symbicort 400/12 Turbohaler
Fobumix 320/9
in BOLD are the inhalers with asthma maintenance and reliever therapy MART License
Special Considerations
Intermittent reliever therapy/Acute asthma
All pMDi’s should be used via a spacer (such as AeroChamber Plus Flow), as this ensures the best drug deposition to the lung and minimises risk of oral candidiasis.
Mild/moderate asthma attacks should be treated with a SABA pMDI + spacer (or MART + spacer) with doses titrated according to clinical response.
SMART (single inhaler maintenance and reliever therapy)
There are currently only three combination inhalers that have a licence for SMART/MART:
Fostair 100/6 MDi
Symbicort (100/6 and 200/6) DPi (licensed from age>12y)
DuoResp Spiromax 160/4.5 DPi
MART therapy should be considered for patients that are non‐compliant with their ICS inhalers and are using large amounts of reliever therapy.
Consideration should be given to the patients’ ability to use either a DPi or MDi (via a spacer) before deciding on a choice of therapy.
Patients on MART therapy do not have a regular SABA reliever inhaler on repeat every month, as the reliever is built into their MART. However, given the occasional need to exceed the maximum total daily dose (often 8 puffs), then a restricted number of salbutamol MDi inhalers per year should be permitted.
Exercise-induced asthma
Immediately prior to exercise, SABA is the drug of choice.
If exercise is a specific problem in patients who are otherwise well controlled with ICS, consider adding one of the following therapies: LTRA, LABA, Sodium cromoglicate or nedocromil sodium, or Theophyllines.
Smoking
Patients who smoke have, in general an increased requirement for inhaled corticosteroids. This is due to a combination of decreased adsorption and also increased metabolism linked to smoking. In this group of patients it is advisable to start at the higher end of the stated range. i.e. Clenil Modulite (beclometasone diproprionate) 400mcg rather than 200mcg.
Monoclonal antibodies and immunosuppressants
Under specialist initiation, immunosuppressants such as methotrexate[unlicensed], and monoclonal antibodies such as omalizumab (child over 6 years for severe persistent allergic asthma) can be considered in children with severe asthma to achieve control and reduce the use of oral corticosteroids.
Non-pharmacological management
Primary prevention
Not recommended: in utero or early life exposure to aeroallergens, maternal dietary supplementation during pregnancy, the use of dietary probiotics in pregnancy.
Recommended: Breast feeding, smoking avoidance, weight-loss if overweight/obese
Secondary prevention
Not recommended: Physical and chemical methods of reducing house allergens, air ionisers
Recommended: Smoking avoidance, weight-loss if overweight/obese, Breathing exercise programmes, Trigger avoidance (including occupational exposure)
Behavioural programmes centred on breathing exercises such as the Buteyko method has been shown to improve asthma symptoms, quality of life and reduce bronchodilator requirement in adults with asthma
Supported self-management (written personalised asthma action plans PAAPs)
PAAPs improve health outcomes for people with asthma.
In adults, PAAPs may be based on symptoms and/or PEF,
with symptoms-only acceptable for children.
PAAP should be provided to ALL admitted patients prior to their discharge.
PAAP should be offered to all patients on ‘active asthma’ GP registers
Monitoring
(At least) annual asthma review should assess:
Royal College of Physicians ‘3 Questions’ (nocturnal symptoms, daytime symptoms, limitation on activities)
or validated asthma questionnaire (ask children directly)Reliever/rescue treatment (more than twice/week or >12 SABA prescriptions/year suggests poor asthma control, >1 MART inhaler per month)
Frequency of exacerbations in previous 12m
Lung function PEF or FEV1 (ideally >80% predicted/best)
Future risk of attacks
Check adherence, inhaler technique and eliminate trigger factors.
Management strategies and supported self-management
Growth in children
Markers of increased risk of future asthma attacks:
Poor current control of asthma
In children: comorbid atopic conditions, younger age, obesity, and exposure to smoking
In adults: older age, female gender, reduced lung function, obesity, smoking, and depression
Asthma treatment in pregnancy
SABA, LABA, ICS, po/iv theophyllines, LTRA, oral steroid courses, sodium cromoglicate and nedocromil sodium, can can be used as normal in pregnancy.
Continuous fetal monitoring is recommended for pregnant women with acute severe asthma.
If anaesthesia is required, regional blockade is preferable to general anaesthesia
Avoid use of uterotonic drug carboprost (prostaglandin F2α) because of the risk of bronchoconstriction.
Women receiving steroid tablets at a dose exceeding prednisolone 7.5 mg per day for >2 weeks prior to delivery should receive parenteral hydrocortisone 100 mg 6–8 hourly during labour.
Use asthma medications as normal during lactation in line with manufacturers’ recommendations.