Diagnosis of asthma
BTS/SIGN Asthma guideline, July 2019
DIAGNOSTIC TRIAD
SYMPTOMS
Wheeze, breathlessness, chest tightness, cough
VARIABLE AIRFLOW OBSTRUCTION
EOSINOPHILIC AIRWAY INFLAMMATION or ATOPY
OTHER FEATURES THAT INCREASE PROBABILITY OF ASTHMA DIAGNOSIS
Triggers: recurrent wheeze with exercise, viral infection, cold air, allergens, emotion/laughter, NSAIDs/Beta-blockers
Variability of recorded PEF and FEV1: lower values when symptomatic compared with asymptomatic
Personal history of atopy: eczema/dermatitis/allergic rhinitis, raised allergen-specific IgE levels, positive skin-prick tests to aeroallergens or blood eosinophilia
Diurnal symptom variability: worse at night/early morning
OBJECTIVE TESTS OF ASTHMA
VARIABLE AIRFLOW OBSTRUCTION
Peak expiratory flow (PEF) charting of variability
More than 20% variability in multiple daily PEF recordings (≥2) is regarded as a positive result for the diagnosis of asthma.
Occupational asthma: serial peak flow four times a day for three weeks at home and at work is a diagnostic test of proven value.
Suitable record forms can be downloaded from http://www.occupationalasthma.com.
Spirometry with Bronchodilator reversibility (BDR) [PREFERRED INITIAL TEST]
May be performed in children aged>5yr
Obstructive spirometry diagnosed if FEV1/FVC ratio less than 70%.
Bronchodilator Reversibility: an improvement in FEV1 ≥ 12% in response to beta-2 agonists or corticosteroids is regarded as a positive result
Challenge Test: direct bronchial challenge test with histamine or methacholine
A PC20 value (provocative concentration causing a 20% drop in FEV1) of 8 mg/ml or less is regarded as a positive result.
EOSINOPHILIC AIRWAY INFLAMMATION or ATOPY
Fractional exhaled nitric oxide (FeNO) testing
Confirms eosinophilic airway inflammation
Test deemed positive (abnormal) if FeNO level ≥40 ppb in steroid-naive adults OR FeNO level ≥35 ppb in children
Approximately 1 in 5 people with a negative FeNO will have asthma (20% False-negative rate)
Approximately 1 in 5 people with a positive FeNO will not have asthma (20% False-positive rate)
Blood tests
Positive if blood eosinophilia ≥ 4%
Raised allergen-specific IgE
MANAGEMENT
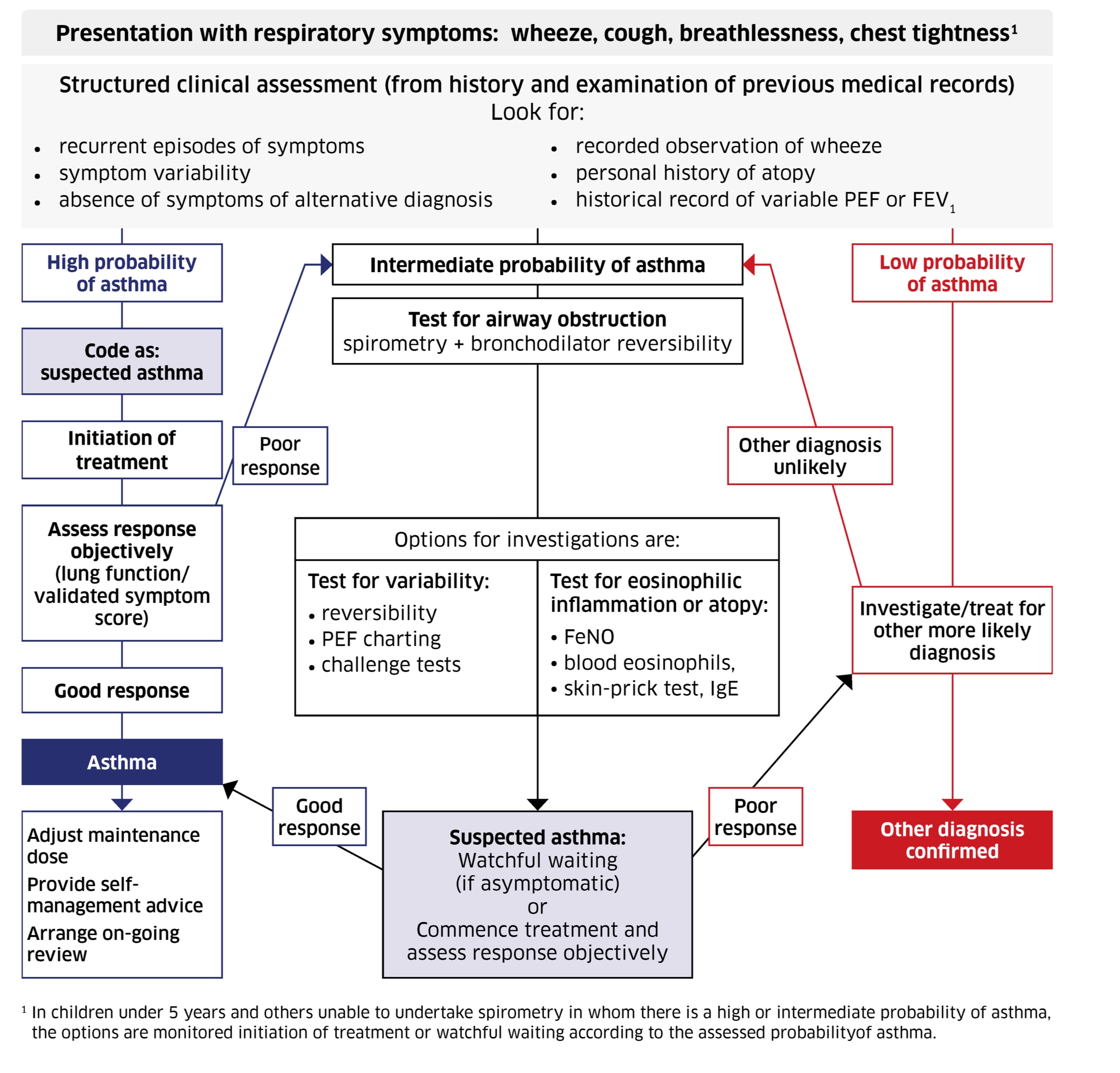
1. HIGH PROBABILITY OF ASTHMA based on symptoms, variability and atopy:
Code as suspected asthma and initiate 6w inhaled corticosteroids + reliever B2 agonist
Monitor and assess response:
Spirometry FEV1/ at clinic visits
Validated symptom questionnaire
Domiciliary serial PEFs with/without symptoms
If good response, asthma diagnosis confirmed and will need adjustment of maintenance dose, self-management advice and on-going monitoring
2. INTERMEDIATE PROBABILITY OF ASTHMA
Undertake OBJECTIVE TESTS OF ASTHMA: variable airflow obstruction (e.g. spirometry with bronchodilator reversibility) AND eosinophilic airway inflammation
Red-flag signs suggesting alternative diagnosis and referral to a respiratory physician
Adults
Severe/life-threatening asthma attack
Prominent systemic features (such as myalgia, fever, and weight loss)
Unexpected clinical findings (such as crackles, finger clubbing, cyanosis, evidence of cardiac disease, monophonic wheeze, or stridor).
Persistent non-variable breathlessness
Chronic sputum production
Unexplained restrictive spirometry
Chest X-ray shadowing
Marked blood eosinophilia
Suspected occupational asthma (symptoms improve away from work) in high-risk occupations
Children
Failure to thrive
Unexplained clinical findings (such as focal signs, abnormal voice or cry, dysphagia, and/or inspiratory stridor)
Symptoms that are present from birth or perinatal lung problem
Excessive vomiting or posseting
Severe upper respiratory tract infection
Persistent wet or productive cough
Family history of unusual chest disease
Nasal polyps
Differential diagnosis
Bronchiectasis: copious sputum, frequent chest infections, a history of childhood pneumonia, and coarse lung crepitations
Chronic obstructive pulmonary disease (COPD): asthma and COPD can be difficult to distinguish clinically and may co-exist. Clinical features of COPD include a productive cough and dyspnoea on exertion in a person over 35 years of age who is a current or previous smoker.
Ciliary dyskinesia: persistent moist cough present from birth.
Cystic fibrosis: persistent moist cough and gastrointestinal symptoms from birth, and failure to thrive in children.
Dysfunctional breathing: breathlessness, dizziness, light-headedness, and peripheral tingling.
Foreign body aspiration: sudden-onset cough, stridor (upper airway) or reduced chest wall movement on the affected side, bronchial breathing, and reduced or diminished breath sounds (lower airway).
Gastro-oesophageal reflux: cough, postural and food-related symptoms, and vomiting
Heart failure: orthopnoea, oedema, history of ischaemic heart disease, and fine lung crepitations
Interstitial lung disease: asbestosis, pneumoconiosis, fibrosing alveolitis, sarcoidosis — dry cough and fine lung crepitations
Lung cancer: cough, haemoptysis, weight loss, or persistent hoarse voice
Pertussis: paroxysms of coughing, vomiting after coughing, or an inspiratory whoop, cough may persist for several months
Pulmonary embolism (PE): acute-onset breathlessness, pleuritic pain, haemoptysis, crackles, and sinus tachycardia
Tuberculosis: persistent productive cough, which may be associated with breathlessness and haemoptysis.
Upper airway cough syndrome: frequent throat clearing and chronic sinusitis or allergic rhinitis
Vocal cord dysfunction: dyspnoea and stridor